
Decentralized Clinical Trials: Why are They Here to Stay?
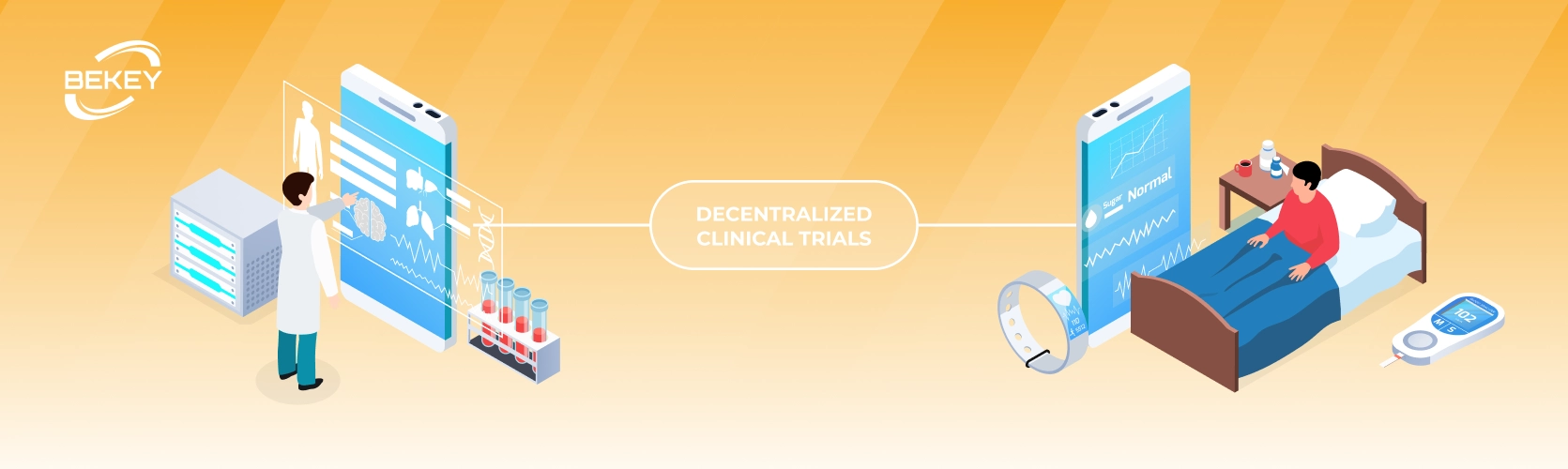
Over the last few years, the idea of decentralized clinical trials has become louder and louder. Both the global COVID-19 pandemic and the growing role of patients in research program development could not help but be affected. According to a survey conducted by Informa Pharma Intelligence, in 2021, due to a pandemic, 76% of researchers were forced to conduct remote decentralized research. Although the term “decentralized clinical trial” can be used in different ways, it is essentially a movement of clinical research away from the front door and offices of medical institutions. In this model, various activities are focused on getting the clinical trial directly to the participant’s home or where it is convenient for him/her.
Why is “Virtually” Better?
Proponents of such an approach as decentralized clinical trials highlight a number of potential benefits.
Patient orientation: they provide convenience and flexibility of the process. After all, a person can participate in the study without leaving home. There is no need to travel or be forced to visit medical facilities — even for the preparation of primary documentation. This is especially useful for patients with mobility problems or those living far from the clinical trial site.
Population diversity: the decentralized research model also allows to expand the geography and demographics of patients. They allow access to a more diverse patient population, as the study has no longer to be confined to a specific medical facility.
Patient maintenance: DCTs significantly reduce moral and financial burden on both patients and caregivers.
“Maturity” of technology: digital health is now fueled by significant investment. And with mobile technology, over time DCTs can collect more data from patients than they do with site visits.
However, decentralization, like most innovations, should not be implemented instantly without proper “training”. “Stakeholders” need to devote sufficient time and resources before they can reap the full benefits. Sponsors need to learn how to implement DCT effectively and flexibly, and support patients and sites on their learning pathways. In terms of regulation, DCTs are in their infancy, so they do not have clearly defined standards. At this stage, sponsors will have to focus on specific priority markets, as well as consider ways to compare the effectiveness of DCT with traditional trials to capture their full value.

Where to Start?
Sponsors may be wondering where to start and where to focus their efforts when looking for an existing software or a developing company for DCT. For them, a combination of business needs and the feasibility of decentralizing certain areas of medicine can be a guide. Some therapies are best suited for digital studies based on factors such as the route of administration of the study drug (oral or infusion), the type of evaluation procedure (non-invasive or invasive biopsy), and whether the patient’s condition is chronic or acute. A team of analysts from ZS (global professional services firm that leverages deep industry expertise — fn) has identified cardiovascular, neurological diseases and diabetes as the most popular areas for DCT, although it can also be used in other therapeutic areas. Oncology and infectious diseases involving digital technologies account for 5% and 4%, respectively. For many therapeutic areas, complete remote mode and decentralization may not be possible or may not be appropriate for patients. Instead, almost everywhere there are specific procedures or analyzes that can be decentralized.
The digital technologies used to collect data vary depending on the study. These may include various wearable/sensory devices, eConsent, electronic clinical outcome assessment (eCOA), electronic health records (eHealth), etc. Mobile technology is often used to replace written diaries with electronic ones and to collect data from wearable touch devices. Home services allow you to collect vital signs such as blood pressure and blood samples.
How is Healthcare Transformated by Mobile Devices?
Whether patients are on short-term or long-term treatment, their mobile devices play a crucial role in keeping in touch with doctors. When the conditions in which people are found make it difficult to travel to the hospital, mobile devices ensure that they do not neglect the necessary support. Thanks to fast registration and in-depth virtual care capabilities, they can share information, ask questions and stay in touch — these are key elements on which effective treatment is based.
Mobile technologies provide instant access to important information:
patient records;
results of analyzes and laboratory researches;
remote monitoring of patients;
communication services such as text, email, and video.
Hospitals often use clinical collaboration platforms, including secure messaging, to streamline communication and access to peer data. Mobile devices, by providing virtual access to these tools, bring the same benefits to home healthcare: increased efficiency, reduced manual processes, and a more convenient approach to care coordination. A 2021 study published in the Journal of the American College of Cardiology found that remote patient monitoring combined with analytics reduced the overall resources needed to care, making them much more effective.
Recently, for example, Google Health presented some developments, according to which smartphones could be turned into tools for disease screening. Innovation could be introduced through telemedicine, saving patients time on doctor’s trips. A feature that allows you to measure heart rate and respiratory rate with your phone’s camera is now available on Android and iOS devices. Another promising way is to use a built-in microphone on the phone as a stethoscope to detect circulatory disorders. Such listening to the human heart and lungs can help clinicians detect heart valve disorders. The possibility of conducting ultrasound examinations with the help of smartphones and, importantly, their decoding for non-specialists is also being studied. DiA Imaging Analysis CEO Hilla Goldman-Aslan said in an interview with “Digital Trends” that such technologies could then act as a second set of eyes for overworked doctors or provide a powerful diagnostic power that was simply inaccessible to patients.
Conclusion - why are they here to stay?
DCT is not a logical, but even a necessary approach and transformation for medicine. However, as with most other updates, in order to reduce risks and provide quality service, connection, and cooperation in the format of “physician-developer-client” is needed. As more providers use mobile solutions to provide care, they must ensure HIPAA compliance to protect medical information. You can read more about this act in our white paper.
Tell us about your project
Fill out the form or contact us

Tell us about your project
Thank you
Your submission is received and we will contact you soon
Follow us
