

Remote Patient Monitoring — a Fad or the New Reality?
Remote Patient Monitoring (RPM) represents a groundbreaking approach that leverages digital technologies to gather medical data from patients across different locations and securely transmit it to healthcare providers for analysis and guidance. This innovative method has transformed the formidable task of remote patient monitoring into an efficient reality.
If your healthcare provider has proposed RPM as part of your health management strategy or if you’re exploring ways to optimize medical care within your organization, you likely have questions about its effectiveness. Does it surpass traditional healthcare practices? Is it a worthwhile investment? In this article, we’ll delve into RPM’s value propositions and how it is poised to reshape healthcare for the better.
Understanding RPM: The Essentials
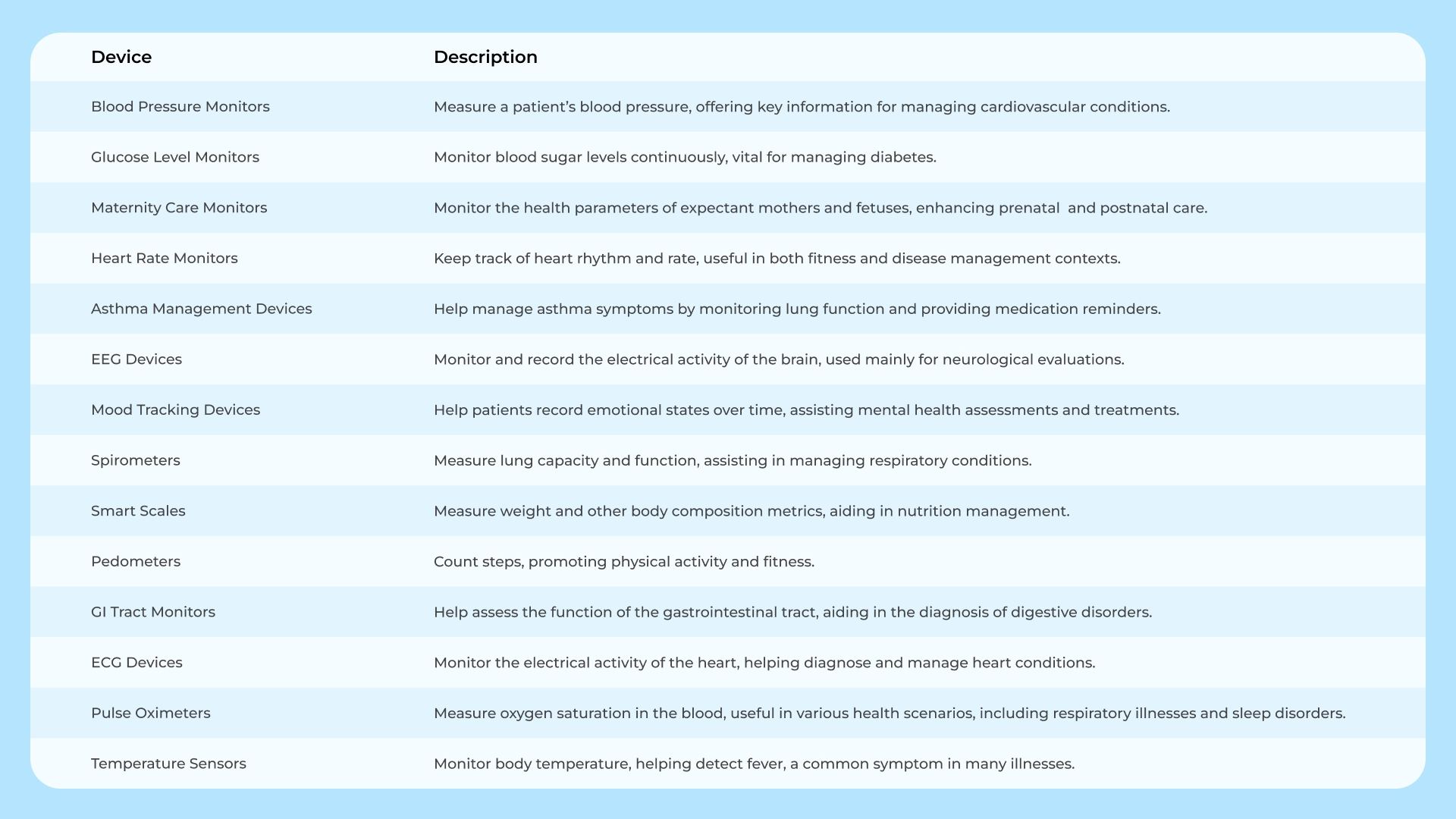
Remote patient monitoring is one of the healthcare trends, empowering healthcare professionals to remotely oversee and manage patients’ health conditions outside traditional clinical settings. This Internet of Things (IoT) network system enables patients to collect health information using medical gadgets or software, which then are sent to their healthcare providers for review, diagnosis, and subsequent treatment planning.
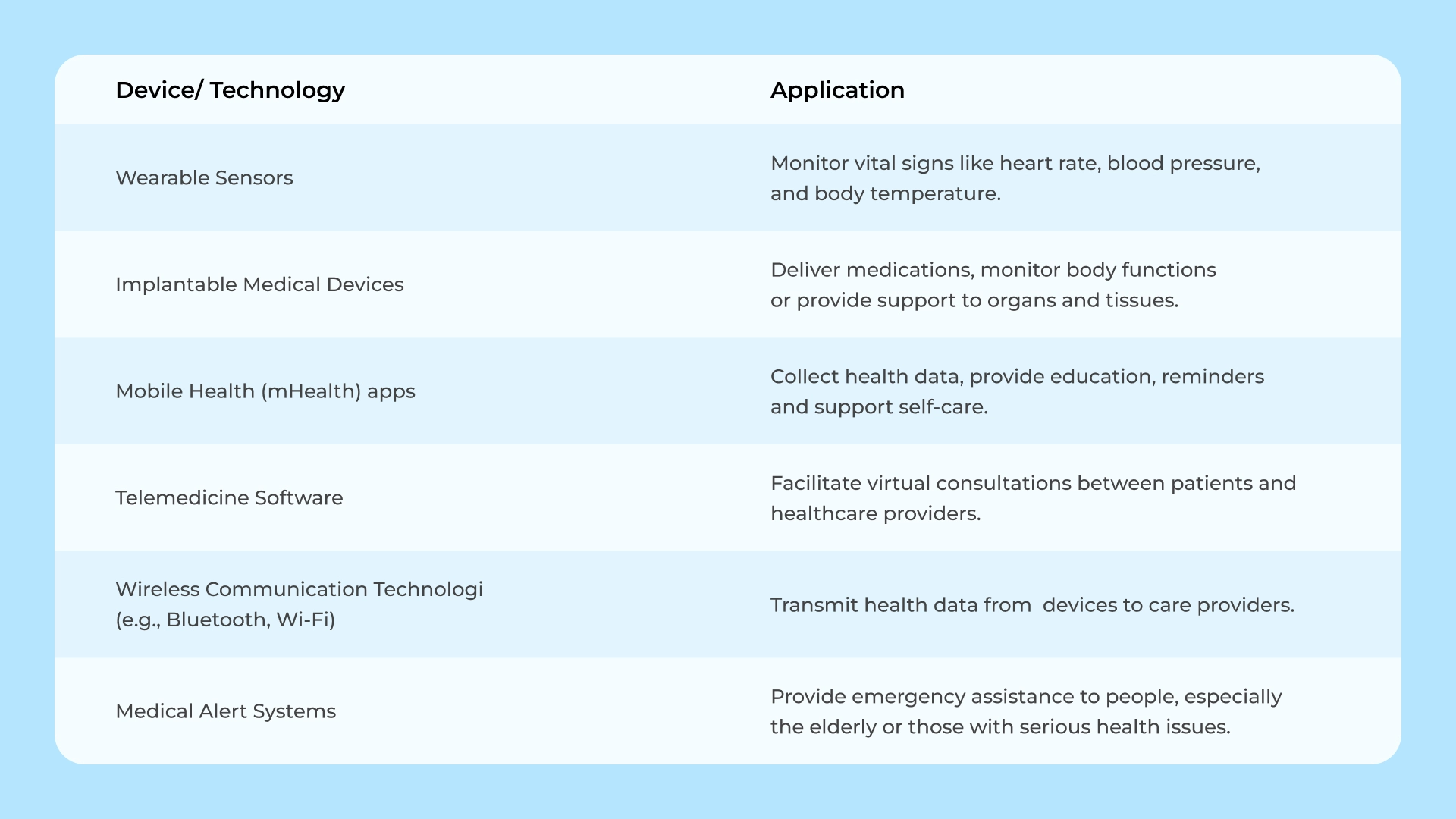
The gathered data is transmitted to the healthcare provider’s system using wireless or internet-based technologies, enabling real-time analysis. Healthcare professionals can utilize this data to track patients’ health status, identify potential health risks, adjust treatment plans, and intervene when necessary.
RPM systems offer significant advantages for patients with chronic health conditions requiring ongoing monitoring and management, as well as older individuals who may have difficulty attending regular medical appointments. Institutions implementing remote patient monitoring solutions experience a remarkable 76% reduction in patient readmission rates, accompanied by an average patient satisfaction score of 89%. These statistics underscore RPM’s tangible impact on patient care and satisfaction.
Exploring the Merits of Remote Patient Monitoring
Insider Intelligence predicts that by 2025, approximately 70.6 million U.S. patients, equivalent to 26.2% of the total population, will be using RPM tools. This substantial adoption rate signals a significant shift toward more digitized and remote healthcare solutions.
According to remote patient monitoring statistics from Research and Markets, the global value of RPM systems is projected to exceed $1.7 billion by 2026, marking a nearly 128% increase. This growth highlights the extraordinary trajectory of RPM within the healthcare landscape.
The competitive environment in the remote patient monitoring market drives tech companies to innovate revolutionary devices, particularly beneficial for individuals grappling with chronic diseases. These devices can be categorized based on the type of device they connect with, their functionality, and their data management approach.
The Advantages of Remote Patient Monitoring
Digital health tools like RPM offer numerous benefits for both healthcare professionals and their patients:
1. Improved Patient Outcomes:
Real-time health updates enable healthcare professionals to identify potential health complications promptly and modify treatment plans as needed, thus enhancing patient health and quality of life.
2. Increased Access to Healthcare:
RPM eliminates geographical barriers, providing access to medical services regardless of patients’ locations, and fostering patient empowerment and control over their health.
3. Reduced Healthcare Costs and Hospital Readmissions:
RPM significantly lowers healthcare costs by reducing hospital readmissions and emergency room visits. Early detection often requires less costly interventions, leading to a more cost-effective healthcare system.
4. Enhanced Convenience for Patients:
User-friendly tools in RPM systems promote patient engagement, adherence to treatment plans, and healthier lifestyle choices. RPM’s remote interface strengthens patient-provider interaction, improving patient satisfaction and care accessibility.
5. Early Detection and Timely Intervention:
RPM tools identify early indicators of potential health issues, allowing personalized disease management and swift intervention, reducing the risk of complications.
How Remote Patient Monitoring Functions
The structure of an RPM system may seem complex, but it essentially consists of core building blocks serving three primary user groups: patients, healthcare institutions, and administrators.
Step 1: Health Data Collection:
Patients activate their health devices, which collect a wealth of information, from heart rate to oxygen levels. This data is transmitted via Bluetooth to a mobile app.
Step 2: Health Data Transmission:
The data is sent to healthcare providers using advanced methods such as the internet, text, or phone, ensuring accuracy and efficiency. HIPAA-compliant (in the U.S.) web applications receive and analyze this data.
Step 3: Data Evaluation and Alerts:
Data is stored in the cloud or the healthcare institution’s data repository. Physicians set threshold values, and deviations trigger alerts, allowing for timely intervention and treatment decisions.
Step 4: Actionable Steps:
Authorities are alerted when urgent medical attention is needed. Physicians communicate necessary modifications to patients, promoting proactive healthcare management.
Implementing RPM in Your Practice
To effectively integrate RPM into your healthcare practice, consider these key steps:
1. Selecting Appropriate RPM Software and Hardware:
Choose tools that align with your existing systems and offer necessary functionalities for remote physiologic monitoring.
2. Empowering Staff with RPM Competencies:
Invest in training and support to ensure your team is comfortable using RPM for patient supervision.
3. Establishing Clear Protocols:
Develop clear protocols for data collection, interpretation, response to alerts, and communication with patients and healthcare providers.
4. Navigating Regulatory Requirements:
Comply with regulatory obligations like HIPAA and state privacy laws to protect patient privacy and data security.
5. Educate Your Patients:
Ensure patients understand how to correctly use RPM devices, emphasizing the benefits of remote monitoring.
6. Assess RPM Effectiveness:
Continuously monitor and assess your RPM system’s impact on patient outcomes and satisfaction, making necessary adjustments for improved performance.
At BeKey, we’re here to support your organization throughout this journey, enabling the seamless integration of RPM into your practice and the delivery of enhanced healthcare to your patients.
In Conclusion
RPM is already realizing its potential, and with industry and public sector collaboration, it can reach new heights. With the right data and a deep understanding of the healthcare landscape, organizations have the opportunity to harness RPM’s promise and drive significant advancements in this dynamic field.
Faq
What is remote patient monitoring (RPM), and how does it differ from traditional healthcare delivery?
+Remote patient monitoring is a healthcare practice that involves using digital technologies to collect and transmit patient health data from a distance. It differs from traditional healthcare delivery by enabling healthcare providers to continuously monitor patients’ vital signs and health metrics remotely, allowing for proactive interventions and reducing the need for in-person visits, thereby improving patient outcomes and reducing healthcare costs.
What are the advantages and benefits of remote patient monitoring for patients and healthcare providers?
+RPM offers patients the advantage of continuous, non-invasive health tracking from the comfort of their homes, leading to early detection of health issues and reduced hospital visits. For healthcare providers, it enables proactive care management, enhances treatment adherence, and reduces the burden of in-person monitoring. Overall, it fosters patient-centric care and a more efficient healthcare system.
Tell us about your project
Fill out the form or contact us

Tell us about your project
Thank you
Your submission is received and we will contact you soon
Follow us
