

Healthcare systems in the USA and Europe: differences, challenges, trends
- The major difference: who pays for healthcare in the USA and in Europe
- American hybrid healthcare system
- Quality of care comparison and challenges in the US healthcare system
- Common challenges: waiting time, regulations, and interoperability
- Now and future trends in European healthcare systems
- Now and future trends in the USA healthcare
- Final thoughts
The amount of money Americans spend on healthcare services is higher than in any of the developed world countries, according to OECD Data. At the same time, only 23% of them think that they get the best care possible — compare this to an average of 70% of satisfaction with healthcare’s quality among EU citizens. Let’s explore this gap.
First, let’s establish a healthcare system “starter pack” — a list of elements, needed to build one.
1. Patients
2. Clinicians and their organizations
3. Payers
Basically, specifics and strategies of healthcare systems in different countries are built around how these three are organized, who is represented in them, and how beneficial in-between cooperation is.
The major difference: who pays for healthcare in the USA and in Europe
An essential of affordability and accessibility of healthcare services, the question of payment is solved differently by Europe and the USA.
European healthcare universal systems
Health coverage in Europe is universal. Having different structures of interactions between insurers, providers, and patients, all European healthcare systems aim to provide care to everyone, on the grounds of free access, equality and equity, and fairness: no matter how much you earn, you’re getting a basic package.
So, the types of universal systems in Europe are:
1. Single-payer healthcare system, where the government or the private sector pays fully for health coverage (so a country/private sector is the main insurer) and the healthcare provider sector is mostly private. It’s mostly free for patients — in Spain, where a single-payer model is used, the very term “spending on healthcare” was declined. Such a system doesn’t imply full-blown governmental control of everything: in addition to the government's funding, there are private insurance companies that still offer coverage for the services of some private practitioners and hospitals’ extra coverage.
2. Multi-payer system, where there is health insurance for people who earn less than a certain minimum and private one for those who earn more. In such a system, patients get free services if they use governments’ healthcare organizations. This construction co-exists with private practitioners and insurers, and a doctor may have a governmental position and hours for private practice. Sometimes, government insurance doesn’t cover some aspects of health plans, required for specific needs, so patients go to private insurers or pay for services out-of-pocket.
Such a two-tier system employed in Germany. Over there, there is a regulation that obliges everyone to get insurance, that is sold by non-profit private companies. There are two types of health insurance (HI): statutory (SHI, they are also called “sickness funds”) and private (PHI). The latter covers few services the former doesn’t, but they are more or less identical. Those who earn less than €56,250 a year covered by SHI, and their not working dependants are included in the plan. Those who earn more or who is self-employed choose between these two. Funds are financed through taxes and contributions. So Germany’s system is based both on the private sector and government.
As you can see, in Europe, universal healthcare systems are often built on the co-existence of private and government funds, which is kinda similar to what happens in the USA. There is, of course, a “but.”
American hybrid healthcare system
Unlike Europe, not all American citizens have access to publicly-funded insurance; government’s funds are available for certain Native American tribes, military families, and veterans. There is also a national health insurance, called Medicare, which covers people over 65 and some people with disability status, people with end-stage renal disease and amyotrophic lateral sclerosis.
Plus, there is a joint federal-state program Medicaid that covers people with low income which expanded under the implementation of the Affordable Care Act to adults, though requiring eligibility income tests. Which means, adults, and sometimes seniors and children, that are supposed to be covered by Medicaid, needed to be proved eligible to get insurance. Each state decides how to organize and run Medicaid, and if the chosen framework is compliant with federal regulations, they get appropriate funds and grunts. ACA also introduced the individual mandate (people had to be insured), but in 2017, it was cancelled.
Most of the healthcare spending in the USA is funded through the private sector: 28% from households, 20% from private companies. Federal funding takes 28%, and local governments pay for 17%. Most healthcare services are delivered privately, even if publicly funded. What does it mean for the state of the system?
It means, first and foremost, that both healthcare providers and insurers can regulate their prices, well, as they want. Which would be a good thing (in the USA, for instance, doctors get higher salaries than in Europe), if it wouldn’t mean that patients have to pay a tremendous amount of money in comparison with other developed countries to be healthy.
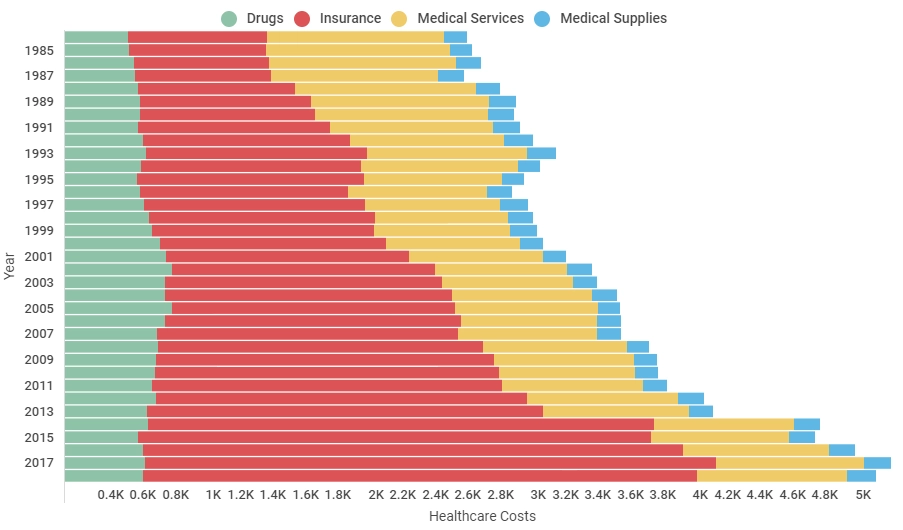
In 2018, the average sum American spends on healthcare became $10.739 per person. Almost half of Americans have employer-provided insurance: in 2018, employers paid 82% of the insurance premium for single coverage and about 67% of the premium for family coverage. Premium is a fixed sum insured person has to pay for the coverage itself, every year, even without submitted claims — though it’s regulated by insurer.
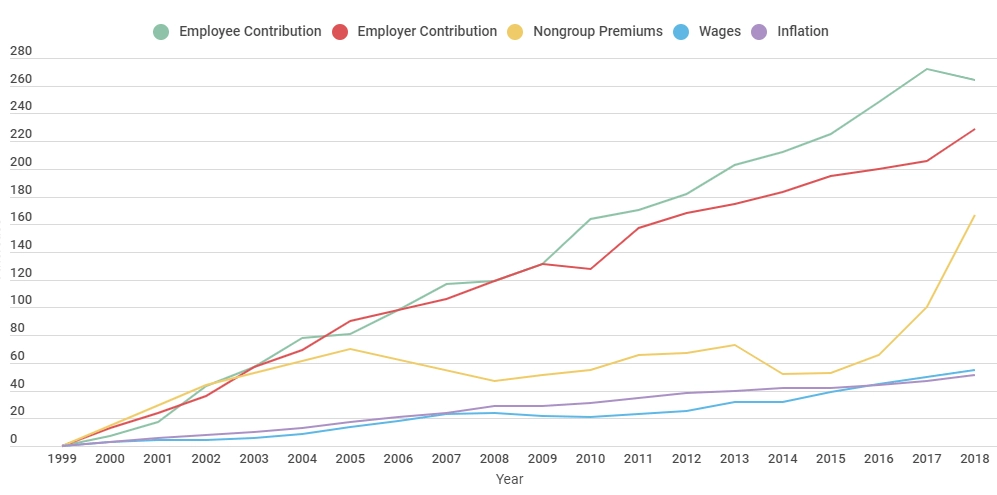
An insured also covers the costs of the visit after the visit, so there is a number of money patients have to pay before it; it is called a deductible. Deductible can be very expensive. Then, there is a coinsurance, a percentage of the cost for healthcare services patients are obliged to cover by themselves. Copayments are what people pay for every visit to a hospital or clinic.
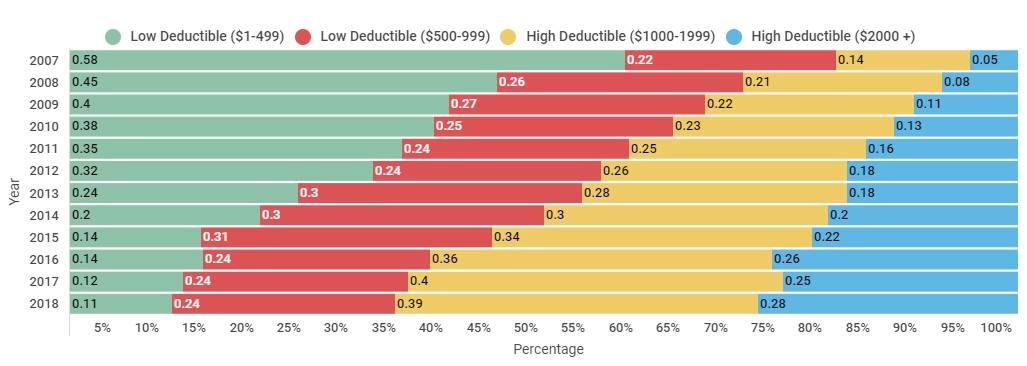
As you can see from the diagram, the cost of both premiums and deductibles are rising with years. There are also a lot of cases where employer-provided insurance doesn’t cover services or prescriptions people need.
Providers, as well as insurers, regulate costs of their services: patients pay for administrative costs (though there is no understanding what exactly is that), providers’ wages, new tech, and other diverse costs that include physicians’ protection from possible lawsuits.
Stories about “Don’t call the ambulance, I won’t afford it” (only 39% of people have enough money to cover emergency visit) and about six litres of saltwater are from the USA.
Quality of care comparison and challenges in the US healthcare system
According to the Health System Tracker data, the US healthcare overperforms in dealing with heart attack and ischemic stroke cases, sepsis prevention, there are fewer deaths from cancers. But, there are issues.
Commonwealth Fund reports show that, while being good in building care processes, the USA underperforms in the domains of administrative efficiency, equity, health outcomes, and accessibility. The high cost of American healthcare is problematic. People with preventable diseases like asthma, congestive heart failure, hypertension and diabetes get to the hospitals more often than in Europe. It’s also more common for Americans to use ER instead of scheduling visits to physicians — a direct outcome of people delaying treatment: one in ten Americans does that. Another consequence of delaying, inaccessibility, and low levels of awareness in population health is higher mortality amenable to the industry: preventable deaths. In particular, they often happen when mental health conditions, substance abuse, and neurological diseases are considered. It’s also harder to adjust to life with a disability in the United States.
In 2018, the number of Americans who preferred to stay uninsured increased — especially among those who use employer-provided health plans. 42% of residents needed to get a second job to pay for their healthcare bills, — which is presumably didn’t improve the overall state of their health. Additionally, Americans pay 203% higher prices for their prescription drugs — and, while European countries successfully negotiate the reduction of costs for meds with drug companies, the USA is yet to find policies and leverage for it.
Among these things, American healthcare providers lead on medical errors and coordination confusion during visits to doctors, caused by the unavailability of patients’ health records and their lab results, which have, in the end, to be duplicated. That is an issue of not usable interfaces of doctors’ electronic systems and, on the higher level, interoperability. While the latter is common both for the USA and Europe, digital interfaces are less efficient in America.
The USA’s health system is at 37th position in World Health Organization rating. There is quite a large room for improvement for it to become truly high-functioning structure: “[it requires] steady financial mechanism, a properly trained and adequately paid workforce, well-maintained facilities, and access to reliable information to base decisions on.” The first 10 include France, Italy, Malta, Spain, and Austria.
Commonwealth Fund states that a way to pursue the US healthcare will be to ensure national insurance coverage (right now, for instance, nearly 29 states have not adopted any ACA’s options), and accelerate and optimize insurance systems, so there is less headache for doctors. Other ways, from our point of view, is to partially restrict providers from balancing insurance claims which don’t cover their services fully. Plus, digital transformation adoption must happen, if the USA healthcare wants to streamline the way it’s operating (and it better be with patients on board.)
Common challenges: waiting time, regulations, and interoperability
Waiting for an appointment time. Universal healthcare systems are often at fault at making people wait for their appointment for months. Essentially, because they are free. But that is a true story not only for European countries like Sweden but for the USA, too: right now, there is a shortage of specialists in almost every industry. This challenge can be addressed through telemedicine or other digital communication methods with patients, evidence-based and clinically-supervised symptom checkers, free education for medical students, and learning & development initiatives within the hospital.
Regulations. Healthcare is a tidbit for cybercriminals because it connects both to money and to people’s personal data, so healthcare providers have to multiply their efforts to protect patients’ data. In Europe, patient data is protected by GDPR, in the US it’s HIPAA, — and countries over both continents are sometimes having a hard time to employ the necessary safeguards.
Interoperability. Considering the fact that the USA has no unified healthcare system, it has different systems to keep the patients’ data too. Which is a large obstacle, if patients, for instance, went to another state and got into an accident: the wait time between getting into the hospital and describing their patient history (if they are capable of describing it) is too great, and it may affect their health badly. EU sees the issue in the lack of interoperability, too. eHealth Digital Service Infrastructure started operating in January 2019: first exchanges, allowed, were ePrescriptions between Estonia and Finland and patients summary exchange between Luxembourg, Czech Republic, and Croatia. EU expects these services to be widely adopted by the end of 2021 — they are already welcomed. The United States has no solution to the interoperable system, yet, but there is hope that through industry collaboration and involvement or large tech players, it will be discovered.
Now and future trends in European healthcare systems
Promote mental health and improve it, as mental health issues are one of the largest causes of deaths over the globe. Moreover, there is a high cost of mental illnesses for businesses, and there is a plan to reduce cases of them by awareness campaigns, reducing stigma, and providing consumer-facing solutions that help people to connect. Same goes for the cases of substance abuse and for establishing more healthy eating habits. Generally, there is a continuous shift from healthcare to wellness in the perception of how healthcare systems in European countries must operate.
Improve care for the ageing population, and the EU is planning on doing so by strengthening community care and implementing more technology to make healthcare accessible and promote healthy ageing habits. These methods are also used to prevent hospitalization of people with chronic conditions.
Reduce healthcare spendings and allocate wasteful spendings in the industry. These are, for instance, the cases of unnecessary hospital admissions, discharge delays, and overuse of caregivers’ services. As well as the previous two, this trend is shaped by adopting strategies of meeting patients where they are before they go to the hospital. Plus, a lot of healthcare spending can be reduced via data analytics that helps providers make better decisions about the way of providing treatment. Thus, better preventive care and data-based decisions are of value.
Reducing waste and prevention strategies partially overlap with a trend for continuously improving, optimization, and establishing more resilience in healthcare systems, as well as the steady promotion of people-centred care.
As we’ve mentioned, Europe continues to expand Electronic Medical Records adoptions and ePrescribing services. Digital technologies in the pockets of healthcare providers are considered to be a way to achieve better long-term care, by the analogy of caregivers being connected to their patients. Their routine tasks, though, will be streamlined (or even automated) via digital interfaces, leveraging eHealth and mHealth applications to help doctors provide truly value-based, personalized services.
Now and future trends in the USA healthcare
American landscape is a bit different. Industry leaders strive for industry consolidation and want to see the value-based care approach adopted and implemented to optimize costs, both for patients and providers.
As one of the methods to do so, while providing healthcare to rural areas that have difficulties in accessing care, the USA widely adopts telehealth and other virtual care solutions.
There is, as well, increasing involvement of physicians in the process of transforming care: they are tired of wasting time in inefficient interfaces, for one thing. The majority of healthcare employees in America want to master data science, AI and robotic process automation to reduce the burden of repetitive tasks.
American patients, on the other hand, are fond of wearables and mHealth apps and other direct-to-customer digital healthcare products: they’d like to use FDA-approved device of such sorts. This fondness is, in our opinion, is the evidence of increasing consumer demands to control their health better and to understand how it changes under different circumstances.
Along with these things, there is an increase of deals and private businesses involvement in the American healthcare sector: technical vendors start to more actively collaborate with large healthcare providers, helping them reduce costs and improve health outcomes via digital solutions. Collaboration between healthcare providers and new, young businesses in insurance is also rising, as both caregivers and insurers want to overcome affordability challenge.
Final thoughts
The fourth industrial revolution, along with digital transformation and people’s generations change need to be acknowledged and addressed, both in America and Europe. Patient demand to get high-quality, affordable, accessible and personalized services challenges the whole world to rethink the way they run healthcare, or to improve and optimize it, putting people in the centre. So, digital transformation and patient-centricity would be trends both continents will continue to dive into.
Tell us about your project
Fill out the form or contact us

Tell us about your project
Thank you
Your submission is received and we will contact you soon
Follow us
