

Telemedicine: History, Use Cases, and Specifics of Software Development
Healthcare, being a conservative field with lots of regulations around and having extremely risk-averse employees, cautious towards new technologies, was forced to change since the COVID-19 pandemic began. A highly potent virus led the provider organizations to choose between the fear of difficulties that come with digital transformation and their workers’ safety.
At the same time, people who stayed in lockdown didn’t magically stop getting sick and didn’t cure their chronic conditions; doctors needed to reach them more often, faster than ever, as people’s well-being declined considerably in isolation.
In addition, pandemic forced clinics and private practices without emergency rooms to question their ability to survive: the decrease in non-urgent care, caused by people fearing the virus and the absence of means to reach them remotely, led to dramatic financial losses.
Changes became necessary, and telemedicine and telehealth became the tools that helped to apply these changes. Attitude towards remote care shifted: care was care, even transmitted via smartphones or laptops. Governments relaxing the regulations around digital healthcare applications all over the world have also been quite helpful. Viewed with distrust at first, now virtual care is welcomed by patients - and they want to use tech for improving their health more than ever. Such circumstances led to the biggest funding midyear, according to Rock Health’s report.
Telemedicine startups grew three times this year, from $220M to $788M, in comparison to Q1 of 2019. This article covers the history of remote health technology; telemedicine’s different forms and applications; brief tips for digital health startups that want to develop telemedicine software. Enjoy!
Terminology: defining telemedicine and telehealth
There is a mild confusion between the terms telemedicine and telehealth in some parts of media covering the digital health industry. Here’s how we are going to define these two:
Telehealth is a broad term for digital information and communication technologies and services that a) patients use to access their health data and manage their care remotely, b) physicians use to attend to patients on distance and communicate both with them and with each other. Telehealth includes telemedicine, yes, but it also comprises the usage of scheduling software, consumer-centric health applications, and so on. Basically, any technology that allows people to improve their health remotely can be considered telehealth.
Telemedicine, on the other hand, is a service or a medical practice of using technology to deliver care. So, for instance, cognitive-behavior therapy apps would be referred to as telemedicine apps only if there is an opportunity to consult with a human therapist within its features.
Note, that some organizations use telehealth and telemedicine interchangeably and some say the latter is older than former, so it is correct to use “telehealth” for all modern remote healthcare tech and forget about “telemedicine”. Above, is a semantic framework we’ve chosen for this article.
A brief history of telemedicine
The first clinical application of what looks like modern telemedicine is assigned to a Dutch physician William Einthoven (who, by the way, got a Nobel Prize in Physiology for discovering ECG and applying it in his practice). In 1905, Dr. Einthoven was able to record electrocardiogram - heart sounds - and transmit it to his lab through telephone - in 1910, two cardiologists from the USA reported transmission of ECGs that helped them diagnose arrhythmia and hypertrophy. Before, there are records of using the telegraph to coordinate patient transfer in the American Civil War, or phone call from a mother to consult on the condition of her child, and so on.
Sometime later, doctors listened to sounds of the stethoscope over the phone, delivered care services to ship crews through radio, and in 1950, the term telegnosis, an old relative of telemedicine, was mentioned for the first time to refer to the transmission of radiology images. Radiology has been one of the first medical fields who adopted telemedicine.
In 1959, med students of the University of Nebraska watched videos with neurological exams that clinicians have been transmitting across the campus. Connecting universities and hospitals became common, vital practice for consultations, especially in psychiatry and neurology.
Telehealth was obviously remarkably attractive to NASA, who needed doctors to check the health of astronaut; the agency started actively participating in developing and testing new technologies since the 1960s which marks the start of the Mercury program: they helped to test and improve connection protocols through satellite-based telemedicine - and, at the end of the next decade, satellite communication opened telemedicine - remote doctor consultation and medical images exchanges - for American rural areas. For instance, they’ve reached Alaska in 1972 and were able to connect a number of local communities living there to large hospitals. In 1984, the Australian government also set up satellite communication and ran a telemedicine pilot on its basis. Five years later, one of the first studies from the field reported the efficiency of telemedicine and its cost benefits for healthcare providers. Even more, there has been an international project connecting America and USSR via telephone lines, aimed to provide aid to the people hurt by the Soviet Armenian earthquake in the 1988 year.
During the last decade of the XX century, telemedicine grew. Telecommunication evolved dramatically. Quicker mobile connection and the Internet made telemedicine more affordable and productive, and American legislators have also recognized it as a care service. That meant people could get remote consultation as a part of their health care plans, and doctors could charge for providing remote health services.
Early nineteenth mark two things, essential for the further growth of the telemedicine: start of regular investments in private virtual care companies and establishment of large telemedicine networks. It became common for patients sites like care homes to connect to specialty hospitals or providers’ ICU or acute care divisions. Government begun financing telehealth programs that improved the education of health professionals in rural areas and expanded patients’ access to care in the same locations.
Hospitals who wanted to use videoconferencing for remote consultations between each other needed to pay lots of money: the high bandwidth, required to establish normal video connection, wasn’t easy to achieve, and hospitals bought expensive equipment and used ISDN Networks to do so.
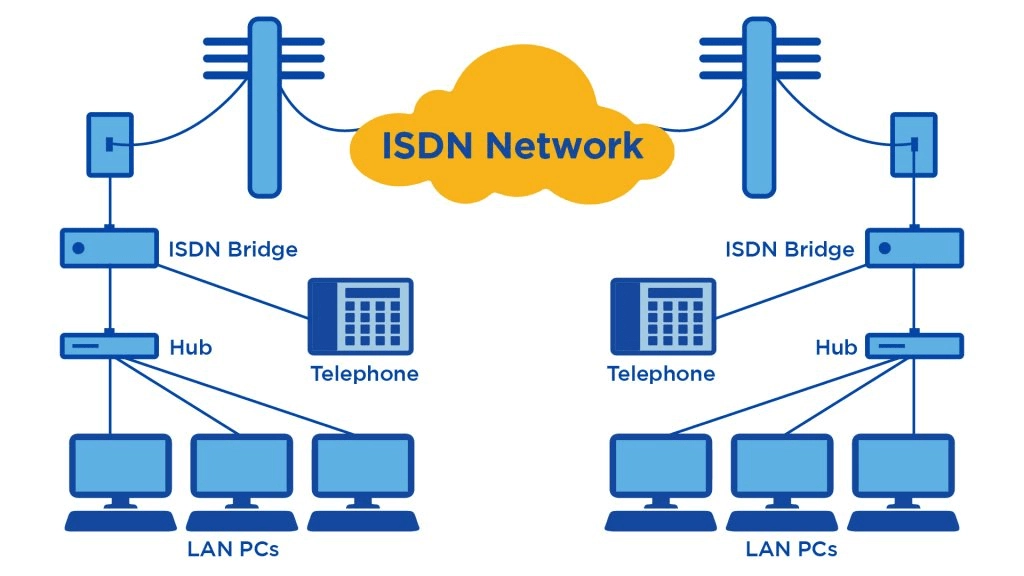
When the first standard that allowed video conferencing over pocket-switched networks have been established, it occurred, providers need to spend a lot of money to adapt firewalls in their system for a new standard - H.232. Those who were willing to transform could pay a fixed price for the Internet without counting megabytes, but, as usual, the majority of hospitals weren’t overjoyed by putting all systems on hold and spending more money. So they held onto ISDN until the end of the decade as it was more reliable.
At the end of 2000s, almost every outpatient service could be provided via telehealth; for instance, delivering of tissue plasminogen activator (iPA) (it restores blood flow to a brain in cases of acute ischemic stroke) become a required, vital operation for provider organizations that didn’t have enough neurologists. ICU, emergency care, and pediatrics started providing via the internet and phone in 2010, as services for children and neonatal care centers have been in the large cities.
The Veterans Health Administration (VHA) who, before 2000, was re-organizing and getting used to the utilization of electronic health records (EHRs), published more than 80 papers demonstrating the clinical capabilities of telehealth. They promoted and utilized telehealth for care homes and chronic disease management. The latter became another leader domain in using telemedicine.
At the end of 2009, healthcare providers needed to implement EHRs if they wanted benefits provided by the government. Installing telehealth was not one of them, but people started rethinking their attitude towards this “expensive, complicated technology,” when more of such technologies appeared. Also, connectivity and Internet access greatly improved, and doctors started using tech for emergencies and natural disaster recovery cases. In 2010, 11 states issued some insurance coverage for medical services.
In the last decade, the number of telemedicine companies increased amazingly all over the world. Telemedicine became the foundation for other digital tech and remote care solutions, created to meet new patient demand for user-centricity and self-monitoring. Telemedicine startups now differ by functions.
Pandemic forced hospitals, technology providers, and governments to complete the shift that has been already happening for a long time: relocate care from hospitals to where patients are.
So, what you can do with telemedicine - or rather, what hospitals, startups, and large healthcare businesses are already doing through it.
Types of telemedicine businesses: applying remote care tech
Virtual consultations
We’ll skip “storages” with healthcare- or therapy-related video by just mentioning them, too, are considered telemedicine, so let’s begin with virtual doctor visits. Among telemedicine services, remote interactive consultations via phone or videoconference are the oldest.
Video-based telemedicine companies deserve to receive lots of attention but know that its popularity differs - for instance, while America loves video calls, Britain prefers telephones and online-requests; NHS reports, less than 1% runs calls face-to-face.
More and more old and new telemedicine platforms - which offer video, chats, voice calls, SMS-based consultations - receive funding and attract attention. One of the oldest telemedicine companies in America, Teladoc, reported 85% of funds growth in Q2 in comparison to 2019. New companies are getting bolder, entering the global market: as Estonian startup, Viveo Health did recently - with free telemedicine for the entire world.
With the evolution of technology, startups also start combining their remote consultation services with other benefits. A startup called Cloudbreak Health offers both telemedicine and integrated language services for people who don’t know English, or understand it badly, or have difficulties with hearing. The platform provides psychiatric and acute care and assistance in case of a stroke. That’s the case for care accessibility, and for moving pass the English-centric essential services.
The pandemic also made almost every large-scale health tech provider consider installing telemedicine features for their offering. One of the largest EHR vendors in America, Epic, partnered with Twilio to launch a telehealth service integrated with their system’s workflows: doctors who use epic will be able to send SMS, voice messages, and SIP channels to talk to patients. DrChrono also recently developed a feature-addition to their own mobile EHR: doctors schedule visits from their calendars - and patients join their appointments from patient portals.
One of the most traditional applications of virtual consultation services is treating chronic conditions: chronic pain, mental health disorders, and so on. A study performed within Kaiser Permanente’s initiative figured that online cognitive behavioral therapy sessions combined with participants’ usage of Noom’s self-monitoring app successfully reduced one of the bulimia’s symptoms - binge eating. Another, more recent study, showed that the usage of wearable sensors and the assistance of personal physiotherapy coaches helped people reduce knee pain and lower-back pain that lasted three months before the start of the program.
Remote monitoring telemedicine startups
Now that we’ve mentioned the application of wearables as an aiding tool in telemedicine programs, let’s talk about them a bit more.
First and foremost, wearables are a source of constant data flow that can be processed and analyzed in real-time mode. That gives several opportunities to improve care both for patients and for doctors.
Doctors can notice abnormalities and react to them quickly, possibly even before they are escalated in the worsening of conditions. Doctors are protected, as they can monitor what’s happening to patients without actually making content and risking getting sick - that’s the factor that has become essential in the pandemic. They can also use this data to create personalized treatments and recovery programs, analyze and adjust patients’ reception of medications and therapies, and, in general, improve the accuracy of care and increase patients’ satisfaction by being with them instantly if they need it.
For patients, wearables are an opportunity to manage their conditions, which gives them a feeling of control and reduces anxiety.
Remote monitoring can also be conducted without wearables: patients can use self-tracking tools and report the changes in their mood, sleep, pain levels, and so on by themselves. Solutions for remote monitoring typically incorporate different notification mechanisms that remind people to take their medication on time, renew their prescriptions, remember about their exercises, and so on.
It’s incredibly efficient: according to the study, conducted for Sony’s mSafety Wearable Platform Division, almost 90% of Americans agreed they could better manage their chronic disease with remote monitoring.
Self-testing services
Wearables are often associated with safety concerns - and it is for a good reason, - but there are more and more cases where telemedicine companies allow connecting their users’ profile to users’ wearables. Some of them can not only measure patients’ vitals but also help them run self-exams.
Recently StethoMe, a Polish-based telemedicine company, announced the launch of a new product. It’s a wireless stethoscope that records respiratory abnormalities for patients to conduct self-examination at home. Before that, StethoMe partnered with two European telemedicine companies, MaQuestionMedicale and HomeDoctor, from France and Spain accordingly, so patients who use their services could access the device.
Self-testing is very close to remote monitoring, but we decided to separate the two, as lately a lot of health tech startups developed or started developing COVID-19 testing kits and offered deliveries in addition to remote telehealth consultations. That’s not another new practice that became widespread in times of social distancing: before, at-home test kits were offered, for instance, from fertility startups and STD health services.
By the way, one of the largest telehealth companies that offer self-testing as a part of their services, Livongo, for diabetes management, recently decided to merge with Teladoc - huge telehealth provider we’ve already mentioned. The deal is supposed to increase access to insulin, Livongo’s devices, and chronic condition management services, delivering them to all Teladoc users needing it.
AI in telemedicine
Telemedicine services enhanced with chatbot assistants are now a part of the hospital and in-home care triage: chatbots collect symptoms and redirect patients to necessary specialty care clinicians, both virtually and in the waiting room. It increases patient satisfaction: the wait time and uncertainty reduce dramatically, - and lowers the load on emergency care nurses and doctors.
In general, AI is often a part of telemedicine offering: for instance, for at-home self-diagnosis, later confirmed or dispelled by a virtual visit to a real doctor - or for therapy, as apps for depression often have two conversation options - users can talk to a chatbot or can schedule a therapy session.
Provider-to-provider consultation
Finally, telemedicine applications are useful not only for people who live in rural areas and have no quick access to proper care services but also for doctors who work there. As radiologists have been using prototypes of telehealth to consult with specialists from universities about CT images, right now doctors from rural areas can contact their colleagues from cities or universities through care coordination platforms to discuss particular cases of diseases. Case in point, recent Oncoshot and MyDoc partnership allowed oncology patients and their doctor to reach out to other oncologists for a second opinion about their diagnosis.
That’s a prospective area for the development of affordable communication software, as urban centers are often bitter about the quality of healthcare in the “faraway places.” As they often have little or no communication with them, they’re mostly operating on stereotypes about rural medicine. With proper lightweight platforms, an opportunity to talk and share knowledge will increase the quality of patient care and physicians’ satisfaction with their work dramatically.
Development of telemedicine software: tech considerations & challenges
From the first glance, one can say everything you need to build a good telemedicine product is to create a patient portal with video connection - and you couldn’t be more wrong.
For once, telemedicine is a healthcare service and it’s covered by government regulations, demanding security of patient data. Since the telehealth boom was caused by pandemic, telehealth companies became one of the prominent targets for cybercriminals - especially if they’ve used third-party services (as Zoom.) You’ll need appropriate safeguards to prevent leaks and theft and protect records of patient visits and other patient information.
Secondly: suppose your telemedicine platform includes remote monitoring function or/and analytical engine (e.g., as a part of an integrated clinical decision support system), and you want to make it connectable to different EHR and EMR vendors. Then, you need to standardize the data for healthcare use. For instance, some data sharing standards in clinical settings include HL7 v2.x and v3 for clinical, administrative, and financial information transfers, DICOM for medical images, CDISC for data from clinical research, and so on.
Make sure your software supports interoperability and communication between doctors and actively avoids ambiguity. A doctor who delivers initial diagnosis or health assessment via virtual appointment and a doctor who runs an at-home checkup later should use the same semantic constructions for descriptions of illnesses, medications, and so on. Leave a place for elaborate notes and encourage their use with UI elements. That’s a distinct challenge for all healthcare software, and useful telemedicine apps are no exception.
The critical nuance for telemedicine software is that it should be platform/channel-agnostic. Different people prefer to talk on different platforms: for instance, 39% of American physicians organize visits by phone, and 40% use the Internet. It seems that a platform-agnostic system seems the best fit for virtual appointment software.
Finally, telemedicine’s primary goal is to decentralize healthcare and increase its accessibility and affordability, which is why you need to adopt technologies that will perform on high levels using minimal network resources. You also need to design your telemedicine app or a platform with accessibility practices in mind - if you want it to be used comfortably by, for instance, senior people.
Conclusion - history of telemedicine
So hey, pandemic makes every participant of the care delivery process reconsider their views of usage of virtual care, and that’s pretty obvious.
Some startups even began to pivot in the telemedicine field by repurposing their initially technological products for the healthcare industry - among them, VR startups, Microsoft and their video calls platform, and so on. Pivoting into healthcare is a serious responsibility and an excellent way to help, so if you think about repurposing, read more about the industry, the way stakeholders make decisions there, and prepare to invest a lot in security.
Telemedicine, as it occurred, works wonderfully not only for managing chronic conditions and acute cases but also for routine, casual visits to doctors. Telemedicine is viewed as convenient and cost-efficient both by patients and doctors, so design your software to align with this view.
Apart from that, now that lots of small local practices lost a lot of money with the pandemic, it becomes apparent that telemedicine services might be a necessity for healthcare organizations.
It’s an opportunity, both for businesses who want to work in the healthcare industry - or are already working there, and want to expand their offering, and for clinicians wishing to deliver better care.
Two years ago, research showed that the most wanted digital feature for patients was the ability to schedule appointments and check symptoms over the Internet. In 2020, it’s clear that receiving care at-home via telemedicine also became the essential demand.
Tell us about your project
Fill out the form or contact us

Tell us about your project
Thank you
Your submission is received and we will contact you soon
Follow us
