

Checklist: Developing Healthcare Wearable Tech
Earlier, consumers adored step trackers and Fitbit-alike bracelets, — and now they more and more use wearables to monitor their heart rate and other vital signs. We’ll tell you a bit about technology and programming beyond wearables and will elaborate on why is it such a challenging thing: to get wearable right, to make it usable and reach its audience.
Hardware for healthcare wearables
A small device, often in the form of a wristwatch, is usually one of the hardest parts of a wearable device to develop (the other is algorithms for data analysis). Often, vendors are ordering hardware from popular sensor providers like Texas Instruments, instead of developing their own solution. Such order largely increases the future cost of the product and makes first sales very hard, especially if there are no additional features except for simple monitoring of vital signs. Low power usage and highly performative processors are a must for any wearables to maintain continuous data stream.

Also, it’s important to think from the start about the comfort of users: the smallest, lightest wearables with strict functionality and, possibly, some engagement mechanisms are the best. A lot of users abandon a wearable if it is uncomfortable to wear. Byteflies, in their Sensor Dot solutions, is using Thermoplastic Polyurethane (TPU) to attach to users: it’s a light material for sensors that is used while manufacturing smart clothes and even touchscreens. ATLASense’s remote patient monitoring solution we’ve developed software for uses Polymonitor that easily attaches to people’s torso.
Connectivity
While developing or ordering hardware for healthcare wearables, think about how it will connect to your computer and application. Demand to keep energy heads low is present here, too. Small, lowly powered batteries require sufficient and light connectivity bridge. The usual solution for that is Bluetooth Low Energy (BLE)— a wireless technology that enables the connection between data, “sensed” by a wearable, and PC or application it is connected to. By the way, BLE is also used in beacons: people install these devices in airports and supermarkets to track people flows and provide brand app’s users with recommendations and directions.
Solutions for raw data processing
In a nutshell, the main function of any wearable tech is to collect, differentiate, analyze and compare to a customized norm wearers’ data and, then, offer them insights. Raw data, collected via wearables, transforms into data points that are transmitted to a server or a cloud in EDF format or deleted automatically.
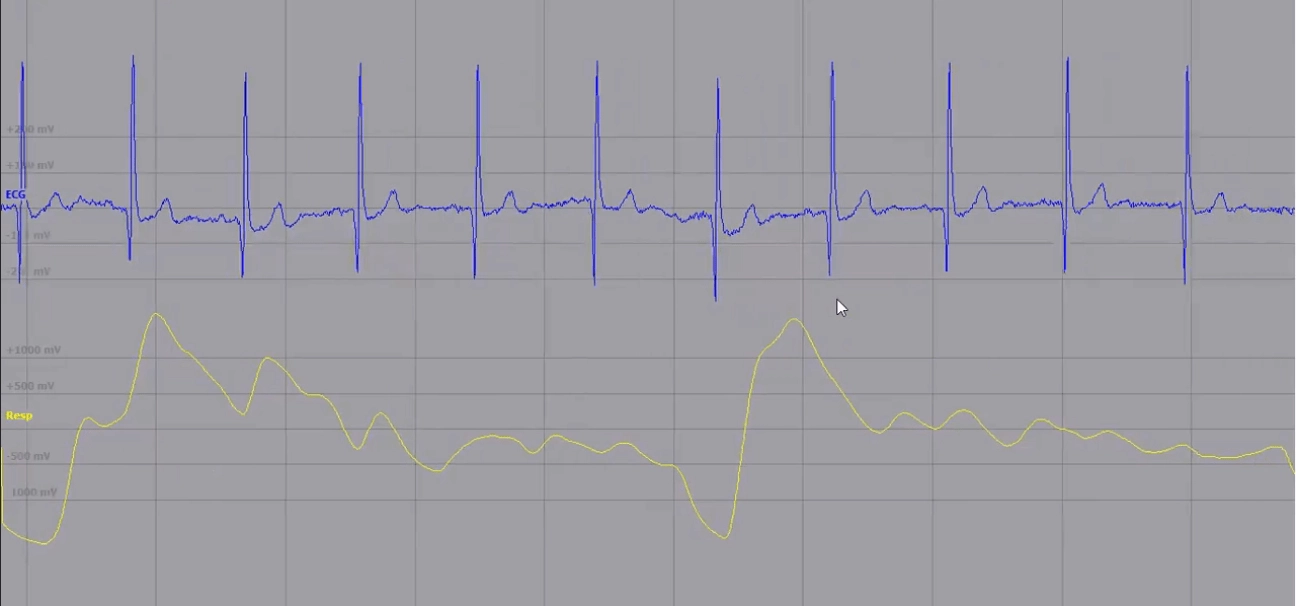
The picture you’re seeing above is a screenshot from this video: there, a doctor analyzes what’s going on at the graphic in terms of patients’ physical health. Meanwhile, at the programming side of these events, raw data is analyzed by Matlab’s formulas and visualized. If you’re an experienced specialist that knows exactly what patient is behind these curvy guys, it’s pretty good. If you’re a patient, not that prominent. That’s why dashboards for clinicians and apps for both groups of end-users were developed.
To find patterns, analyze and apply different formulas and models to raw data, data scientists use Matlab (as a most high-level tool, that is also used by physicians and scientists), R and Python (as separate programming languages that require an understanding of their syntax in particular and how programming works in general).
These languages allow applying algorithms to time series (time series is a set of data points, composed in a sequence of events) to analyze them and forecast, on the basis of obtained data, the future behavior of a data flow. In our case, time series can represent patients’ respiratory activity, heart rate, blood sugar levels, etc, — and forecasting would help healthcare specialists and vendors to predict increases and decreases in the probability of certain health outcomes.
Creating a mobile application for wearable device
As we’ve already mentioned, a mobile application is a tool that helps patients to really understand data. In the article on healthcare scheduling application, we described how to design one of the three features that are most wanted by healthcare end consumers: online booking. The ability to see, analyze, and, generally, be in control of one’s data is their second desire, but only 11% of digital healthcare solutions give them that option.
So, to put patients in control of their data and connect medical staff to a real-time data stream, you need to provide first ones with a usable, understandable, and actually helpful app, and give the second ones the same clear UX on their desktop dashboard (and an app). In an app case, you need to transform algorithms and formulas from your data science software (Matlab, R, Python) into a programming language that is supported by smartphones. It can be Objective-C and Swift for Apple and Java for Android, or other compatible languages. Alternatively, you can build a cross-platform solution through Flutter, React Native, or Xamarin.
For the ATLASense case, BeKey “translated” Matlab formulas and syntax in C and C++. Then, via JNI — it’s an interface that allows working with a code written in C and interpreting it for Android environment — we rewrote and adjusted functionality for an Android application. To enable real-time data monitoring on mobile, too, we applied OpenGL library to visualize life signs and made sure functionality, written in C, constantly “shares” fresh data with Android’s Java environment, simultaneously analyzing them.
Mobile features for patients
The very main idea of value-based care is to provide services to patients on their terms. To do that in wearables and applications that are connected to them, you should provide insightful, helpful information on how they can improve their health; what all these graphs mean; what to expect. It’s quite useful to add input forms on factors that can affect the data you’re collecting: if you’re measuring heart rate, for instance, you can repetitively ask users about their level of physical activity, alcohol consumption, medications, smoking habits, etc. For remote health monitoring solutions, it’s also useful to add “emergency button” patients can hit any time they don’t feel well, and connect them to an available provider in a given medical area or even notify the ambulance.
Mobile features for doctors
As we’ve said, data is only useful if it’s used. Using machine learning algorithms, a system can understand whether a patient might be in a crisis and notify nurses. It was a super-important feature for ATLASense because the solution was targeted at elderly people who often live alone and, if something happens, might not be able to call ambulance themselves. Via smart notifications, doctors start to receive information that allowed them to plan check-ups and more or less prepare for emergencies.
Interoperability
If your wearable devices would be used in a hospital, it’s better to store the patient data in the cloud and connect it to a hospital’s EHR: 49% of all mHealth app publishers were doing it last year. Note, that despite the fact it’s a very costly feature (takes at least two third of your app development budget), integration with EHR is a prospective idea. Data transferred from wearables might become a source of food for healthcare analytical engines and AI algorithms.
Also, if you don’t plan to create a mobile application, it’s better to leave the device’s API (Application programming interface) open, so they could connect to FDA-approved medical app and add value in other ecosystems and apps as well. Interoperability slowly becomes new normal for mHealth landscape. For users, it means an ability to, again, control and share their patients’ records, which is good for their engagement and product satisfaction, which is, subsequently, good for referrals and for your revenue. And if you plan an app, know, that mHealth solutions with open API are more profitable than those without, according to Research2Guidance.
Overcoming challenges in healthcare wearable tech
Good news for vendors and for healthcare providers: if they make real-value data actionable, people will have meaningful information about their health that will definitely improve their well-being and their image of patient care. Not really good news for the same pair: nowadays, physicians are struggling to make sense of real-time data and positively affect clinical outcomes. So, in terms of remote monitoring of patients’, wearables are pretty hard to utilize. Why?
First of all, because healthcare — like other industries — suffers from a lack of tech specialists that will help them create algorithms for data analysis. And even if a wearable device is of high-quality, there’s no way for doctors and nurses to quickly get how complex algorithms work. The solutions are, of course, hiring data scientists that are experts in healthcare and implementing corporate learning initiatives, that will provide hospital staff with explanatory, actionable training. Also, adoption should be smooth: you can’t throw new technology on people who’ve been using fax for communication for the last 30 years and expect them to get used to it in mere moments.
Secondly, it’s a market strategy (lack of it). Vendors create a wearable nobody wants, and even get investments because they’re passionate and can talk beautifully, but it occurs their device is heavy, expensive, or its sensors aren’t accurate. And not accurate sensors for wearables can mean only “garbage in — garbage out” — people can’t possibly obtain patient care insights from it. The solution is user research. There’s never enough research.
The third is security. As you know, any healthcare solution that interacts with patients’ data must be HIPAA-compliant and FDA-approved. That’s one side. From the other side, low-quality engineering and low-quality data can lead to rather dire consequences — especially in terms of devices that monitor chronic and life-threatening conditions. So, if something is wrong, no regulations’ approve for the wearable. The solution is, of course, experienced tech talent and quality engineering.
And, finally, marketing. The rising popularity of Apple Watch and somehow unquestionable leadership of Fitbit on the market of healthcare and wellness wearable tech is a clue that vendors need a brand and communication strategy from the very start. Otherwise, you’re at risk to waste a lot of resources — and, after device’s release, you’ll have to wait until people will find out about you.
As a conclusion, we’d like to say this: every serious healthcare project should stand on the solid scientific ground of clinical studies. Without them, everything else is pretty much useless. And they will eat a lot of your time, no matter what you’re creating, wearable patches or superlenses. Your stage of scientific and user research might also be your stage to start talking about yourself. Start thinking about the application of your technology both for providers and patients. And don’t think that you must hurry in terms of software development: when you’re dealing with people’s health, it’s better to take your time and pay attention to details.
Tell us about your project
Fill out the form or contact us

Tell us about your project
Thank you
Your submission is received and we will contact you soon
Follow us

